Navigating Ethical Issues in Telenursing: Balancing Patient Care and Digital Boundaries
As healthcare becomes increasingly digitized, telenursing has emerged as a vital component of telemedicine, providing accessible healthcare advice and support over the phone. This approach, popularized in countries like Sweden, has made healthcare more accessible and efficient. However, telenursing also presents unique ethical challenges, often surrounding issues like privacy, autonomy, and integrity. In this blog, we’ll explore the ethical dilemmas in telenursing, why they arise, and the need for ethical competence in this evolving field.
The Rise of Telenursing
In recent years, telenursing call centers have expanded significantly in Sweden, allowing patients to access healthcare advice 24/7 through a national helpline. This model is similar to services like NHS Direct in the UK, where trained nurses provide guidance on health concerns, from infections to chronic conditions. For many patients, especially those in rural areas, telenursing offers a lifeline to healthcare support without requiring in-person visits. Yet, the virtual nature of this service introduces ethical complexities unique to telenursing.
Common Ethical Dilemmas in Telenursing
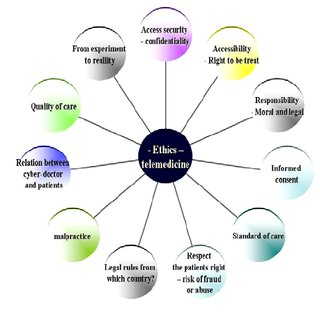
Telenurses face ethical challenges that are distinct from traditional nursing due to the nature of remote communication. Key ethical issues in telenursing often include:
1. Autonomy vs. Beneficence
- Telenursing often involves communicating through a third party, such as a family member calling on behalf of a patient. This can complicate respect for the patient’s autonomy, as the nurse may not be directly engaging with the individual receiving care. Striking a balance between honoring the patient’s wishes and acting in their best interest, especially when they are not the direct communicator, is a core ethical concern.
2. Privacy and Confidentiality
- Handling sensitive patient information over the phone raises concerns about privacy and confidentiality. Unlike in-person visits, where confidentiality is easier to maintain, telenursing risks exposing private information to unintended listeners, whether in the patient's environment or the nurse’s setting. Ensuring data protection and secure documentation is a persistent challenge in telemedicine.
3. Integrity in Information and Documentation
- Effective documentation is vital in healthcare, and telenursing is no exception. However, the virtual environment can lead to gaps in documenting patient interactions, as telenurses rely heavily on verbal information without physical observation. This raises ethical concerns about the accuracy and completeness of records, impacting patient safety and care continuity.
4. Prioritization and Resource Allocation
- With high call volumes and limited resources, telenurses must prioritize cases based on urgency, which can create ethical conflicts. Making swift prioritization decisions without in-person assessment is challenging and may inadvertently compromise care for those in lower-priority situations. Balancing efficient resource use with patient-centered care requires nuanced ethical judgment.
5. Responsibility and Information
- Providing accurate information without inducing unnecessary worry is a delicate balance. Telenurses must ensure patients understand their health situation and the recommended actions while managing their concerns. Ethical issues arise when trying to provide honest guidance without causing harm through fear or misinformation.
The Role of Ethical Competence in Telenursing
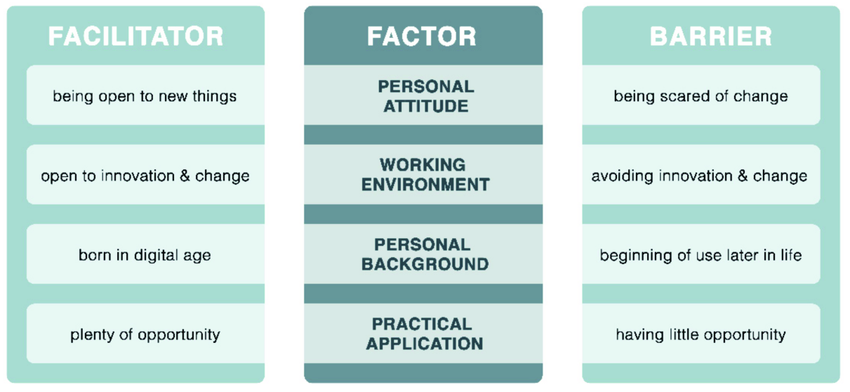
Given these challenges, ethical competence is crucial for telenurses. Unlike traditional nursing, where non-verbal cues and in-person context aid decision-making, telenurses rely solely on verbal information and may face ethical dilemmas with limited data. Developing ethical competence can help telenurses navigate these dilemmas with confidence. Key areas of focus for ethical competence in telenursing include:
- Training on Privacy and Confidentiality: Telenurses need robust training on safeguarding patient data in a virtual setting, including best practices for secure documentation.
- Understanding Autonomy in Remote Care: Balancing patient autonomy with beneficence becomes complex over the phone, especially with third-party callers. Ethical training on autonomy is essential for informed decision-making.
- Regular Ethical Discussions and Case Studies: Discussing real-life scenarios within the telenursing team can help practitioners reflect on their approaches and make informed choices when faced with ethical challenges.
Conclusion: Building an Ethical Framework for Telenursing
While telenursing has brought convenience and accessibility to healthcare, it also requires heightened ethical awareness and skill. To provide safe, effective care, telenurses must navigate ethical concerns such as autonomy, privacy, and prioritization thoughtfully. Building ethical competence through training, open dialogue, and ongoing education can support telenurses in meeting the unique demands of remote healthcare. As telemedicine continues to grow, fostering a strong ethical framework within telenursing will be essential to ensuring that quality care is balanced with respect for patient rights and well-being.
4o